Far infrared therapy for arteriovenous fistulas
Far infrared therapy for arteriovenous fistulas
Timothy Shipley, Debbie Sweeney, Iain Moore, Sean Fenwick, Hatem Mansy, Saeed Ahmed.
City Hospital Sunderland NHS Foundation Trust
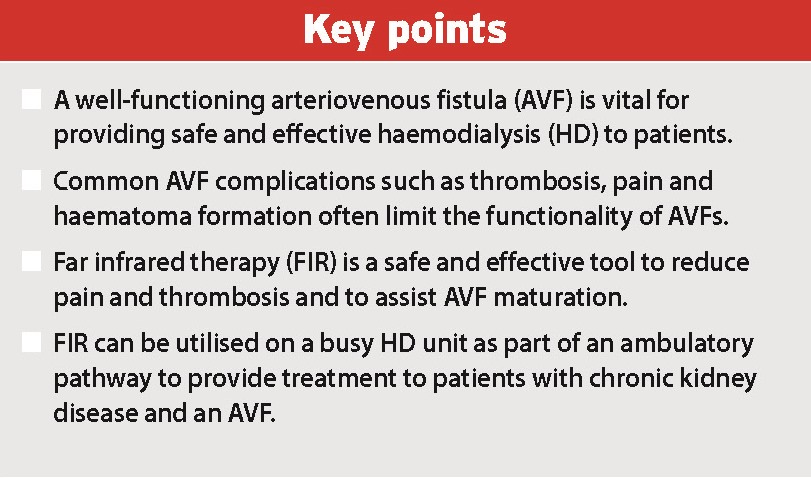
Reliable, safe and effective vascular access is the Achilles’ heel of haemodialysis (HD). It is widely accepted that a functioning arteriovenous fistula (AVF) is the best form of access for HD; this is reflected in the fact that there will be a future target of 85% for the number of prevalent patients dialysis via an AVF in UK HD units. When compared with AV grafts and dialysis catheters, AVFs are associated with a lower infection rate and, therefore, reduced patient morbidity, mortality and length of stay in hospital. Dialysis adequacy is also superior via and AVF, leading to improved patient well-being and quality of life. For these reasons, it is highly desirable that a patient already has a functioning AVF established when they start HD. Equally, it is vital that these AVFs are well maintained and continue to function efficiently throughout a patient’s time on HD.
A common reason for failure of an AVF is thrombosis. Reduced blood flow through an AVF increases the risk of thrombosis and this is often caused by AVF stenosis, usually at the level of the venous outflow. Adequate blood flow through an AVF is also necessary to achieve sufficient clearance of small solutes, with a blood flow of 250-500ml/min being desirable. Improved blood flow through AVFs and a reduction in the rate of AVF stenosis will, therefore, improve dialysis adequacy and enhance patient outcomes. Novel treatment strategies to achieve these goals are being explored.
Far infrared therapy
Infrared is invisible electromagnetic radiation with a wavelength that is longer than visible light. It can be subdivided according to wavelength into near infrared (0.8-1.5μm), middle infrared (1.5-5.6μm) and far infrared (5.6-1,000μm). There is increasing evidence that infrared radiation has beneficial effect on tissue healing and endothelial function, which has led to its use in the treatment of skin necrosis and wound healing. The application of far infrared therapy (FIR) to AVFs in HD patients has been studied as a way to improve fistula blood flow, thereby reducing complications of fistula thrombosis and improving dialysis adequacy.
FIR is a safe treatment. A40-minute sessions is associated with a rise in skin temperature to 38-39℃, without causing the skin irritation of burin injury sometimes associated with other types of thermal therapy
FIR appears to benefit AVF function through both thermal and non-thermal effect. Infrared radiation is sensed as heat by thermos-receptors, with an increase in temperature of up to 4℃ at a depth of 10mm when applied to skin. This has a vasodilatation effect, which improves blood flow through the fistula.
The non-thermal effects of FIR on AVF function are achieved via its effect on the vascular endothelium. FIR increase heme oxygenase-1 (HO-1), an enzyme and an important regulator of endothelial inflammation. HO-1 induction reduces platelet aggregation and vascular smooth muscle growth, creating a less thrombogenic surface within blood vessels. FIR, therefore, reduces vascular inflammation through HO-1 induction. It does so in a time-dependent fashion, such that the greater the length of FIR exposure, the greater the amount of HO-1 induction. A randomized controlled trial by Lin et al demonstrated improved blood flow rates and a reduction in AVF malfunction in HD patients treated with FIR. They hypothesized that the benefit were due to the anti-inflammatory properties of FIR.
The Sunderland experience
FIR for AVFs was introduced to our renal unit in December 2008. Initially, it was used to help maintain AVF function by treating haematomas and pain on needling. We found FIR an effective treatment in this clinical setting and have presented data on this area at international nephrology meetings.
FIR has now been adopted into a systematic programme of treatment for our predialysis and HD populations at City Hospitals Sunderland NHS Foundations Trust (CHSFT). Patients are treated immediately after AVF formation with three FIR sessions per week. FIR continues for an average of six weeks. Doppler ultrasound is used to measure AVF flow rate and an assessment from the multidisciplinary team determines if the AVF has matured sufficiently to enable efficient HD, or if further surgical or radiological intervention on the AVF is thought necessary. Figure1 outline the protocol at CHSFT for the application of FIR to new AVFs.
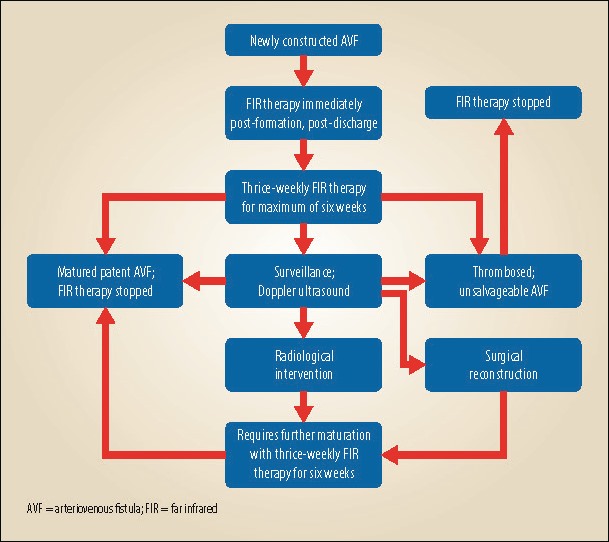
FIR can be continued for a longer period of time if future development of the AVF is thought to be feasible. It is an extremely well-tolerated treatment, with no side-effects reported by any of the patients undergoing the treatment at CHSFT.
Between January 2011 and April 2012, 1,272 individual FIR sessions took place at CHSFT on 139 patients – 903 for HD patients and 369 for predialysis patients. The average number of treatment sessions per patient was just under ten. Patients attended the renal outpatient department at the hospital three times a week for their treatment, which takes place in a dedicated room next door to the HD unit under the management and supervision of a team of specialist renal nurses.

The flexibility of the treatment allows in-centre treatment during dialysis, clinic visits or inpatient admission, or treatment at home using a portable device (see Figure 2).
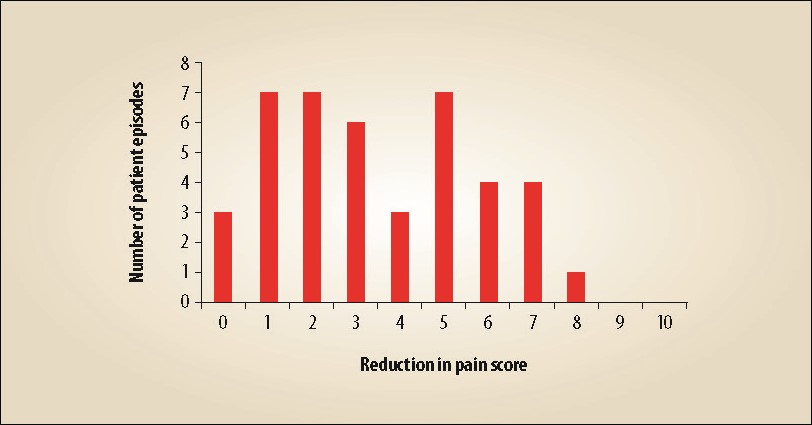
Patients have objectively recorded a reduced pain score on needling an AVF under the influence of FIR, as well as improvement in haematoma resolution. We surveyed 40 patients on our HD unit who underwent FIR of their AVF because of pain associated with needling (see Figure 3). Patient testimonials have been integral to developing our service further.
Conclusion
The creation and preservation of AVF is vital to ensure the best possible outcomes for HD patients. However, the high rate of complications associated with this process pose a significant challenge. FIR is a safe and effective treatment modality that has been shown to reduce these complications and improve the efficiency of AVFs through its direct anti-inflammatory properties.
At CHSFT, we have shown that it is possible to set up a dedicated, nurse-led FIR service within a busy dialysis unit, which is available to all patients with CKKD who have AVFs. Our experience and feedback from patients informs us that it is a well-tolerated treatment that reduces pain for patients during needling, and has the potential to improve patient outcomes by optimizing their HD treatment through better vascular access.
—————–British Journal of Renal Medicine 2013; Vol 18 No 4, P30-31

